Missing a hospital outpatient appointment can delay recovery and rehabilitation, as well as being costly to the NHS and preventing someone else from being seen.
For these reasons work was carried out at Edenbridge and District War Memorial Hospital, to see why some patients staying there for a short time, after being discharged from acute hospitals, were nearly missing their outpatient appointments at other hospitals and clinics – and to see how improvements could be made.
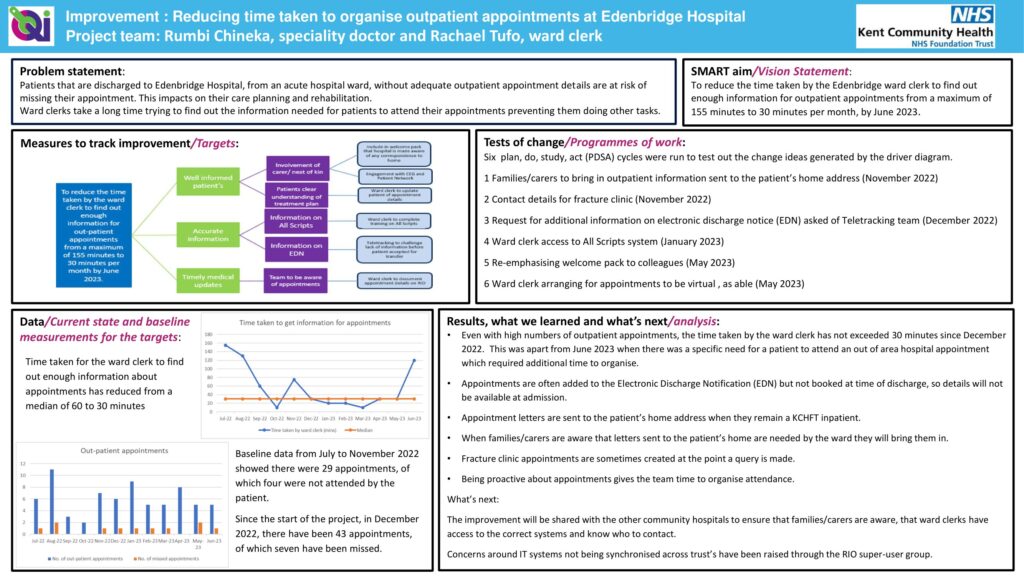
The aim, at Kent Community Health NHS Foundation Trust (KCHFT), was to make things better for patients, in line with the trust’s We care strategy and to reduce the time the ward clerk was spending chasing outpatient appointment information. On occasions, it could take up to two hours to track information down, for just one person.
With some, the issue was that appointments were being sent to home addresses, when the person was in hospital. The patient and colleagues at Edenbridge hospital were then reliant on family, friends or neighbours picking up the post and passing the information on.
Speciality Doctor Rumbidzai Chineka and ward clerk Rachael Tufo, who led the work, also found clearer information on the electronic discharge note would help, along with the different systems used by hospitals and healthcare providers being able to share information better.
The pair put a number of changes in place. These included:
- asking families and carers to share information which had gone to a home address
- asking acute hospitals to add more detailed information to the electronic discharge note
- the ward clerk having access to a range of patient information systems
- the ward clerk arranging for some appointments to be carried out virtually, where possible
- community hospital staff knowing who to contact at acute hospitals regarding outpatient appointments.
The work was carried out between July 2022 and July 2023.
Dr Chineka said: “We found that the electronic discharge notice might say an outpatient appointment had been made, but it didn’t say where or when. We would then have to spend a lot of time chasing these details, if the patient did not know.
“The systems we were using didn’t pick up all appointments and we found that some orthopaedic virtual fracture clinics and some specialist appointments did not appear.
“However, since we have made changes, things are now much better and have greatly improved. Another thing that helped was that in the patient welcome pack we added a note to families to let us know of any appointments coming up which they were already aware of.
“We’ve been very proactive, as knowing when appointments are coming up gives the team time to organise attendance.”
Next, the improvement will be shared with KCHFT’s other community hospitals. Issues around there being further improvements to IT systems being synchronised across the trust have been raised with the KCHFT RIO super user group. RIO is the trust’s Electronic Patient Record (EPR system.
The work was carried out as a quality improvement (QI) project. Dr Chineka has previously completed the trust’s QI Fundamentals training. A driver diagrams and plan, do, study, act (PDSA) cycles were used to help with the project, as well as there being support from QI advisor Robyn Shelmerdine.
Find out more from the project on a page, below:
The reducing time to organise outpatient appointments project on a page


