Parents can be more assured than ever that their children are in the best and safest of hands when they visit a minor injuries unit or an urgent treatment centre in Kent, thanks to the introduction of a system which quickly identifies babies and youngsters who might be seriously unwell.
The system is used widely in large hospital accident and emergency departments and Kent Community Health NHS Foundation Trust (KCHFT) was keen to see if it would work just as well in smaller settings.
The trust decided to trial the Paediatric Observation Priority Score (POPS) and started off with Sheppey Minor Injury Unit (MIU). It worked so well that POPS was then rolled out across the trust, being introduced at Sittingbourne and Edenbridge MIUs and at Sevenoaks, Gravesham, Folkestone and Deal Urgent Treatment Centres (UTCs) too.
POPS is a checklist which quickly scores, between zero and 16, acutely ill children, taking into account a combination of physiological, behavioural and risk factors. This allows staff, even if inexperienced, to assess, prioritise and treat acutely ill children and manage risk in busy clinical areas.
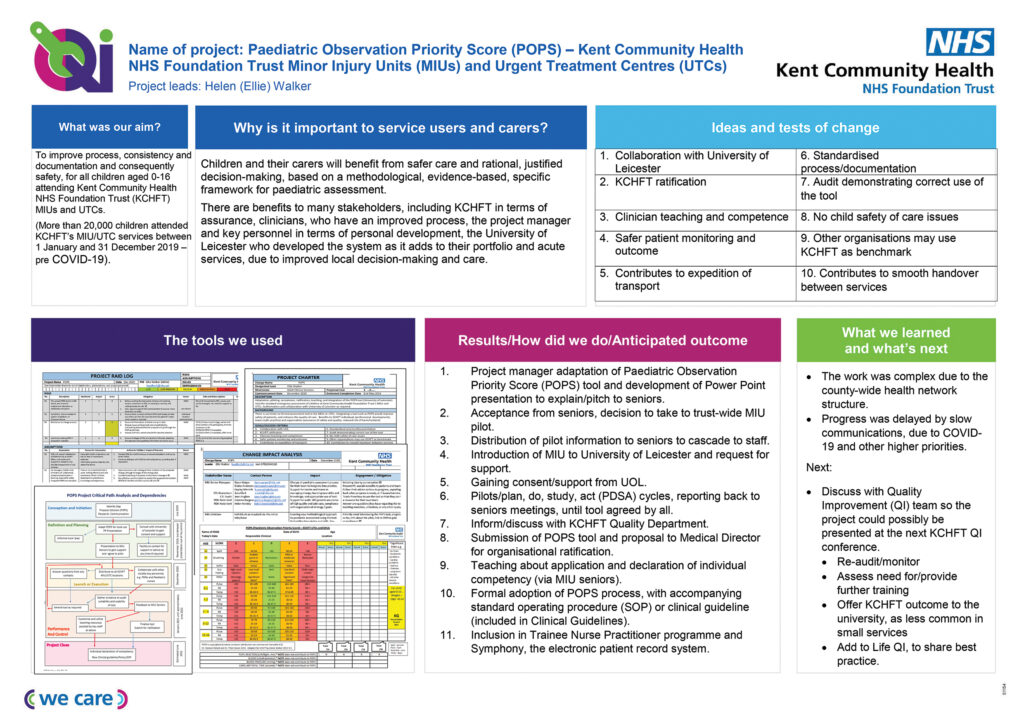
MIU Nurse Practitioner Helen Walker, who is known as Ellie, led the improvement project. She said: “I wanted to improve the way things were done in terms of consistency and documentation and consequently safety, for all children attending KCHFT MIUs and UTCs. During 2019, pre-Covid, there were 20,000 children attendances, so a large number.
“We were using a vital signs and a scoring tool which was designed for adults, but we didn’t have one specifically designed for children, so I looked into this further.
“POPS has been used for some time in emergency settings, but it’s effectiveness in smaller settings is still largely unknown. I took a good look at it and another similar tool and came to the conclusion that POPS was the best one for us, if I could adapt it to suit our precise needs.”
Ellie, who is on a temporary secondment to KCHFT’s quality improvement (QI) team, worked closely with the system’s founders at the University of Leicester to trial the system at KCHFT and is reporting results back to them.
She said: “Using POPS results in improved patient safety for children that come into our centres. Decision making is methodological and evidence based and follows a specific framework for paediatric assessment. It’s a system emergency services were already using, so it helps us work together better.
“We implemented it in one MIU, tested it, reviewed it and adapted it. Once we had it right, we rolled it out across all seven centres, following staff training in how to use it.”
Ellie set up a project team and used a QI approach on the project. QI is used by healthcare trusts and others around the world and looks at how things are working and how they could be done better. QI is a methodology and set of tools which can be used to address problems. Ellie used the plan, do, study, act (PDSA) tool on the project to continually review and adapt the POPS system, so it would meet the trust’s specific needs.
The improvement project ran from January 2020 until January 2021. Following senior management approval, roll out of the new system began shortly after, although there were delays to the planned programme, due to COVID-19.
The effectiveness of POPS will continue to monitored, along with any further staff training which might be needed.