A project, which aimed to improve a dietetic service for care home residents who need nutritional support, has resulted in patients being discharged quicker and increased staff capacity.
A review by the Community Dietetic Team within Kent Community Health NHS Foundation Trust (KCHFT), indicated that some residents were staying on caseloads for a prolonged period of time. The project looked to see if things could be done differently, so that patients could be discharged sooner, while also making sure patients would still receive quality care. It also wanted to make sure dietetic staff time was being spent in the most efficient and effective way.
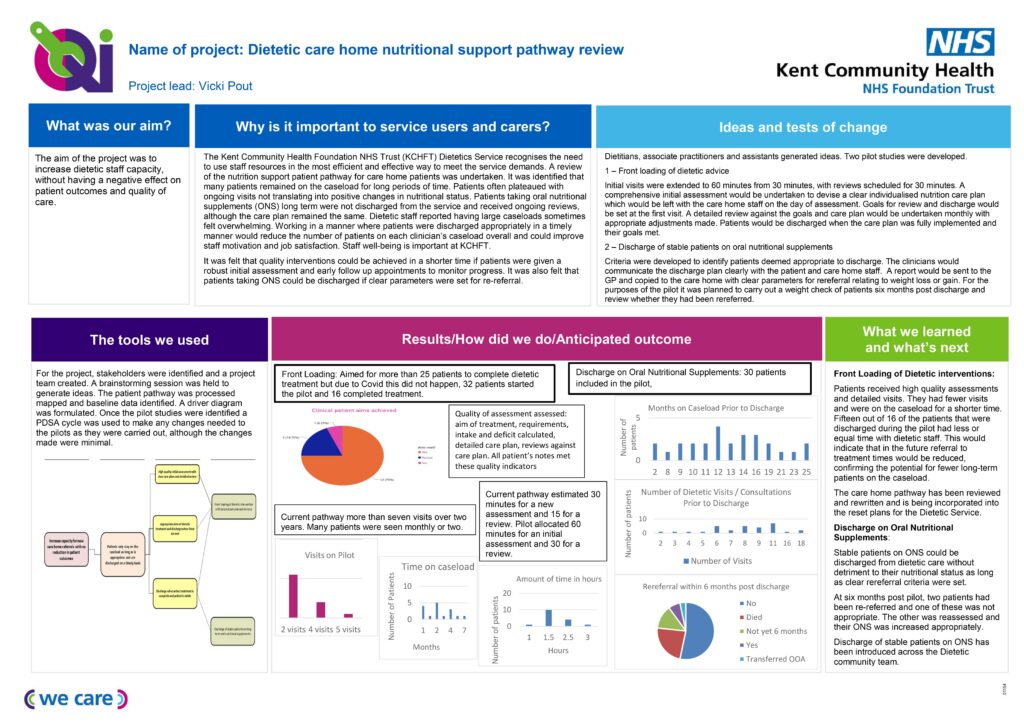
Two pilot studies were set up involving 30 patients each. The studies tested various changes to see what would lead to an improvement.
The findings were that patients having an intensive initial assessment, clear goals being set from the outset, regular reviews and discharge of patients with clear parameters for re-referral, would all help.
Vicki Pout, Professional Lead for Dietetics at KCHFT, headed up the quality improvement (QI) project, with the aim of releasing dietetic staff time and increasing capacity for new care home referrals, with no reduction in patient outcomes. Ideas for making improvements were generated from a group of dietitians, associate practitioners and dietetic assistants.
Vicki, pictured, said: “I wanted to make sure patients only stay on caseloads as long as is appropriate and are discharged in a timely manner. We need to use our staff resources in the most efficient and effective way to meet the demands of the service and the benefit of the patients.
“To improve the way we worked, we needed the patient pathway, for those referred by care homes for nutritional support, to be reviewed. We found a high-quality initial assessment made a big difference, along with discharging patients when their active treatment was complete.”
The pilot studies took place between September 2019 and April 2020. One looked at front loading of dietetic advice by extending initial visits from 30 minutes to an hour with a comprehensive initial assessment, developing a clear, individualised nutrition care plan and goals, along with a meal plan. The care plan and meal plan would be left in the home on the day of the visit rather than being typed and sent at a later date. Regular monthly reviews were scheduled to look at and amend the care plan and assess whether the aims of treatment had been reached.
The other pilot concentrated on patients taking oral nutritional supplements (ONS). In this pilot, patients who were stable and needed ONS to meet their nutritional requirements, were discharged with clear parameters for re-referral.
Vicki said: “Both pilots resulted inpatients remaining on caseloads for less time, resulting in a reduced number of dietetic visits and dietetic time. A review of patient records showed no detriment to patient outcomes or quality of care. The new ways of working are being introduced across the team.”