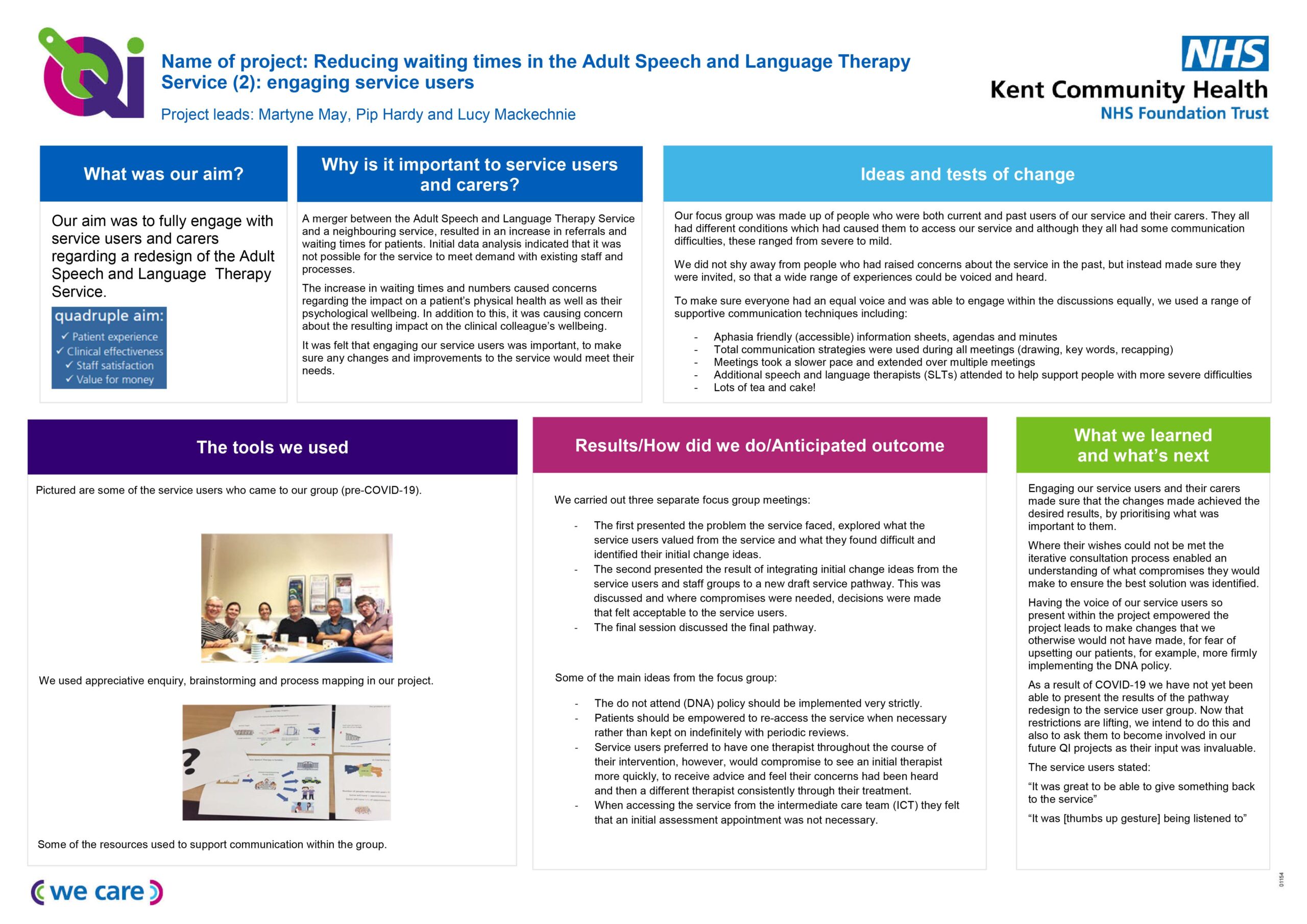
Asking patients what is important to them was at the heart of a project to make improvements in the Adult Speech and Language Therapy Service at Kent Community Health NHS Foundation Trust (KCHFT).
Meetings were held with a group of patients to gather their views, with the group including those who had significant language difficulties. This meant supported conversation techniques were needed during the meetings, which included using short sentences, highlighting key words and using pictures to help understanding.
In the sessions, there was an explanation of how the service worked and was funded. The issues facing the service were discussed, as well as some ideas for change that had been gathered from clinicians and administration colleagues. Everyone’s ideas were used to see how things could be done better.
The quality improvement (QI) project, led by Martyne May, Adult Speech and Language Therapy Quality Lead, aimed to improve how patients moved through the system.
It resulted in reduced waiting lists and waiting times across Kent, which had a knock-on effect of staff feeling less pressured. Martyne was helped at the patient meetings by speech and language therapists Lucy Mackechnie and Annette DeLooper, who gave additional communications support.
Martyne said: “We had ideas about what we could do to change the design of the service, but we wanted to know what our patients thought and what mattered to them. Top of the list for them was being seen quickly and always seeing the same therapist.
“We explained why there were sometimes long waits and why seeing the same person isn’t always possible and discussed finding possible compromises. I went back to the clinical and the administration teams and explained what would work for our patients.”
Martyne involved all stakeholders from the start, including the administration, management and clinical teams, as well as people who use the service. As a result, a new way of working pilot was trialled in Canterbury.
The old process saw the team prioritise referrals as high, medium or low risk, based on information gained from referral documents. They would be placed on a waiting list and seen in chronological order. The patients could be seen by any member of the team, who would work with them until they were ready to be discharged.
As a result, the team had to juggle their continuing therapy caseloads with the new referrals. This resulted in patients who had an immediate physical risk, perhaps developing a pneumonia as a result of difficulty in swallowing, being seen quicker than someone with communication difficulties, who might have to wait longer because their physical risk was not as great, even though their mental health may have been a concern.
The team decided this was not the best way to do things.
The new process saw all patients receive an initial, one-off appointment where their needs could be fully assessed by a clinician, they could receive immediate advice and support and they were then added to a treatment waiting list, based on clinical needs. For some patients, this was not appropriate and separate pathways were developed. These included those who needed rapid access, such as patients with motor neurone disease.
Martyne said: “I’d been working on another project, a rapid response dysphagia service, where it had become apparent that having a senior therapist making decisions about clinical need at the start of the patient journey worked well.
“So we introduced this. As a result, at these initial appointments, patients whose needs were best met by other services or who just needed one appointment, could then be given advice or reassurance and be discharged.
“Our prioritisation for therapy is now based on the clinical needs as assessed by an experienced speech and language therapist.”
When the team took a close look at how things were being done, they also found clinicians were spending a lot of time trying to contact patients to make appointments. As a result of the project, booking appointments was streamlined and moved over to the administration team.
The pilot ran from October 2019 to February 2020. A rollout of the changes was delayed by the COVID-19 pandemic, but the new way of working was introduced across the service at the end of 2020.
The project has resulted in:
- reducing all waiting times to under 18 weeks
- reduced waiting list numbers
- clearer patient pathways through the service.
Martyne said: “Although initially there were some concerns from clinicians about the changes being made, once the new process was in place, our pilot team said it did not want to go back to how it was before”.
Martyne is a qualified quality, service improvement and redesign (QSIR) practitioner, having finished her training with KCHFT at the beginning of 2019. The QI tools she used included process mapping, stakeholder analysis, a driver diagram, the sustainability tool and statistical process control (SPC) charts. Her project is on Life QI, a portal where KCHFT QI projects are logged.
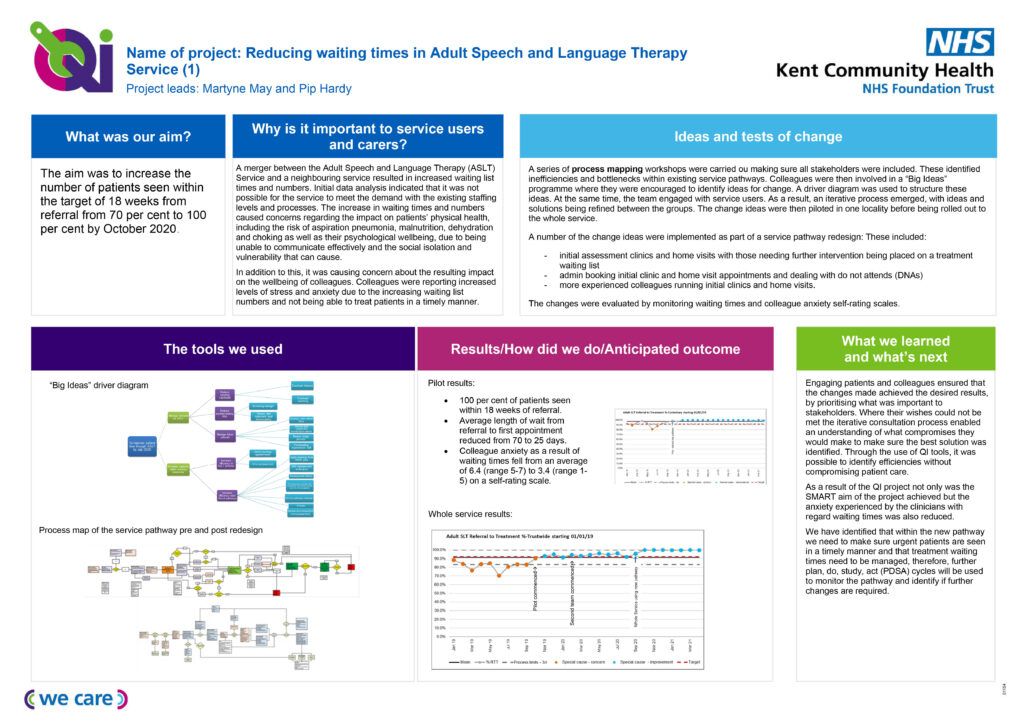
The reducing waiting times project on a page